Hereditary Cancer Risk Assessment: An Overview
Not all cancers are sporadic. While most cancers occur by chance, approximately 5–10% are hereditary, caused by gene mutations passed down through families. These inherited genetic changes can significantly increase the risk of cancers such as breast, ovarian, colorectal, prostate, and pancreatic cancer.
A hereditary cancer risk assessment is recommended if you or your relatives may carry a gene mutation associated with increased cancer susceptibility.

Why Hereditary Risk Assessment Is Important
Early identification of hereditary cancer risk empowers patients and clinicians to take proactive, evidence-based steps for prevention, early detection, and personalised care planning.
Understanding Genetic Risk
Identifies inherited gene mutations that may increase cancer susceptibility and clarifies how these risks are passed through families.
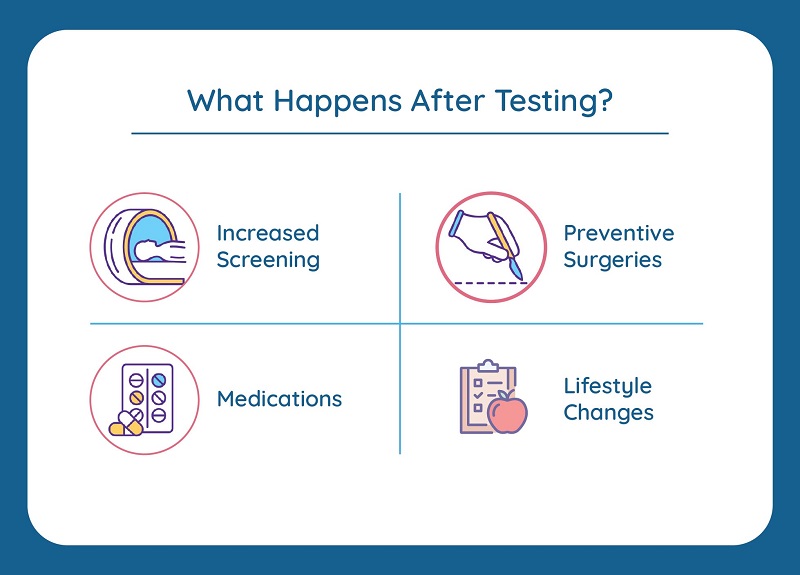
Advanced Screening & Testing
Enables access to specialised genetic testing and enhanced screening protocols for early-stage detection.
Personalised Treatment Planning
Helps clinicians tailor treatment strategies based on genetic findings, improving precision and outcomes.
Structured Medical Surveillance
Establishes regular monitoring schedules for early detection and timely intervention in high-risk individuals.
Preventive & Lifestyle Measures
Encourages preventive strategies, lifestyle modification, and risk-reducing interventions to minimise future cancer risk.
Book a Personalised Genetic Risk Consultation
Take an informed approach to managing your family’s cancer risk. Connect with Dr Aparna for a personalised genetic risk assessment, grounded in clinical evidence and compassionate care.
Genetic Risk Assessment: Is It for Me?
You may benefit from genetic testing for hereditary cancer if you have:
Multiple Affected Relatives
Several family members diagnosed with the same or related cancers.
Early Cancer Diagnosis
Cancer detected at an early age (less than 60 years).
High-Risk Tumour Types
High-risk hereditary tumour types such as ovarian or pancreatic cancer among relatives.
Known Genetic Syndromes
Known hereditary cancer syndromes such as BRCA1/2 or Lynch syndrome.
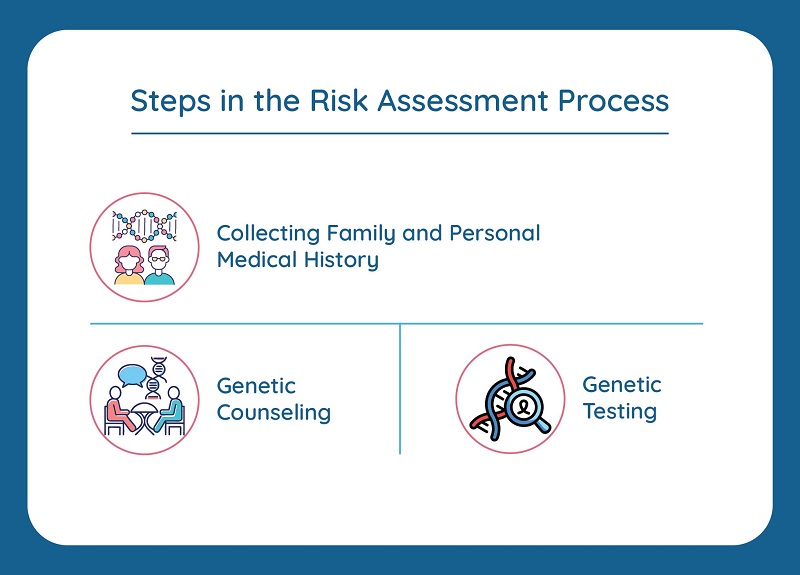
The Process
A structured, evidence-based approach to hereditary cancer risk assessment and management.
Annotated Family Tree
Evaluation of cancer patterns across generations.
Genetic Counselling
Explanation of risks, benefits, and implications.
Molecular Testing
Use of next-generation sequencing to identify mutations.
Personalised Roadmap
Individualised surveillance, prevention, and treatment strategies.
Our Expertise
As a cancer genetics and molecular oncology specialist, I integrate advanced molecular diagnostics with compassionate care. My goal is to ensure that patients and families navigating hereditary cancer risk experience clarity, confidence, and proactive guidance.
Integration of advanced molecular diagnostics with personalised care.
Specialised hereditary cancer testing with focus on accuracy.
Empathy-driven counselling and support for families.
Take the Next Step
Knowledge is one of the most effective tools for cancer prevention. If cancer is common in your family, a hereditary cancer risk assessment should be a priority. Together, we can develop a safe and informed plan for you and your family.
Contact Us to Book Your Consultation